ISLAMABAD, Jan 29 (ABC): Nipah virus is a rare but highly dangerous infectious disease that can spread from animals to humans and, in some cases, from person to person. Although outbreaks are uncommon, the virus is closely monitored by health authorities because it can cause severe illness, including brain inflammation and respiratory failure, and has recorded high fatality rates during past outbreaks.
The disease is classified as zoonotic, meaning it originates in animals and can spill over to humans under certain conditions. Over the past two decades, Nipah virus has caused several outbreaks in South and Southeast Asia, prompting governments and health agencies to maintain surveillance systems and emergency response plans.
What is Nipah virus and where does it come from
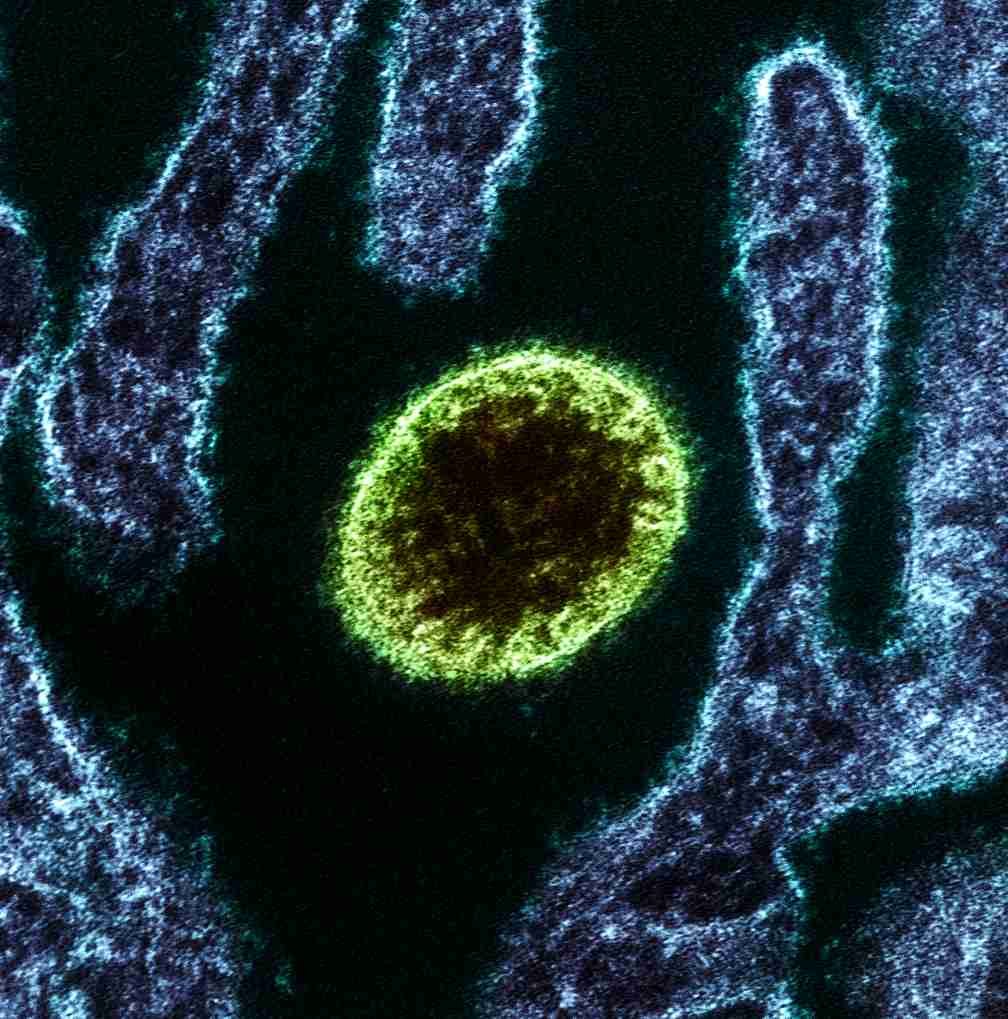
Nipah virus belongs to a group of viruses known as henipaviruses. Its natural hosts are fruit bats of the Pteropus genus, commonly referred to as flying foxes. These bats can carry the virus without showing signs of illness and shed it through saliva, urine, and droppings.
The virus was first identified in 1998–99 during an outbreak in Malaysia and Singapore. In that outbreak, fruit bats transmitted the virus to pigs, which acted as an intermediate host. People who worked closely with infected pigs, particularly farmers and slaughterhouse workers, became ill.
Subsequent outbreaks in Bangladesh and India revealed a different pattern, with infections often linked to contaminated food and limited human-to-human transmission.
Where outbreaks have occurred
Confirmed human outbreaks of Nipah virus have been reported in Bangladesh, India, Malaysia, Singapore, and the Philippines. While outbreaks have been geographically limited, the bats that carry the virus are widely distributed across Asia, the South Pacific, and parts of Australia.
This wide natural range of the animal reservoir means the risk of spillover exists beyond the countries that have already reported cases, particularly in regions where people live or work close to bat habitats.
Symptoms and clinical features
Nipah virus infection can range from mild illness to severe, life-threatening disease. Some infected individuals may show few symptoms, while others deteriorate rapidly.
Early symptoms usually appear as a general viral illness and may include fever, headache, muscle pain, sore throat, cough, and difficulty breathing. Because these signs are non-specific, early cases can be difficult to identify without a clear exposure history.
In more severe cases, the virus affects the brain, leading to encephalitis. Symptoms at this stage can include confusion, drowsiness, disorientation, and seizures. Some patients progress to coma within 24 to 48 hours of neurological symptoms appearing.
Respiratory complications, including pneumonia and acute respiratory distress, have also been reported, particularly in outbreaks involving person-to-person transmission.
Incubation period
The incubation period for Nipah virus is typically between four and 14 days. In rare cases, symptoms have appeared several weeks after exposure. This long and variable incubation period complicates contact tracing and outbreak control.
How Nipah virus spreads
Nipah virus can spread in several ways.
Animal-to-human transmission occurs through direct contact with infected animals such as fruit bats or pigs, or through exposure to their bodily fluids.
Food-borne transmission has been a major factor in some outbreaks. People have become infected after consuming raw date palm sap or fruit contaminated with saliva or urine from infected bats. This type of spillover from animals to humans is known as a spillover event.
Human-to-human transmission has been documented, particularly among family members, caregivers, and healthcare workers. The virus spreads through close contact with respiratory secretions or other body fluids of an infected person. While sustained community transmission has not been observed, clusters linked to close care have occurred.
Who is most at risk
People at higher risk of infection include those who live in or travel to areas with known outbreaks, individuals who have close contact with bats or pigs, and those who consume raw or unprocessed food products that may be contaminated.
Healthcare workers and caregivers are also at increased risk if appropriate infection-control measures are not followed, especially when treating patients with respiratory symptoms.
Testing and diagnosis
Because early symptoms resemble many common infections, doctors consider Nipah virus primarily in patients with relevant exposure histories. Laboratory testing is used to confirm infection, usually while the patient is still ill. Testing may also be performed after recovery for surveillance purposes.
Prompt diagnosis is critical, as early supportive care can improve outcomes and help prevent further spread.
Treatment and patient care
There is currently no licensed, widely available antiviral treatment specifically approved for Nipah virus infection. Care is mainly supportive and focuses on managing symptoms and complications.
Treatment may include rest, hydration, fever control, respiratory support, and management of neurological symptoms such as seizures. Severe cases often require intensive care.
Because the disease can worsen quickly, early medical attention is essential when Nipah virus is suspected.
Prevention and risk reduction
Reducing the risk of Nipah virus infection depends largely on minimizing exposure.
People living in or visiting affected areas are advised to practice good hand hygiene, avoid contact with bats and sick animals, and stay away from areas where bats roost.
Consumption of raw date palm sap should be avoided, and fruits should be washed thoroughly and peeled before eating. Fruit that appears partially eaten or contaminated should not be consumed.
Close contact with the blood or body fluids of anyone suspected of having Nipah virus should be avoided unless proper protective measures are in place.
Infection control in healthcare settings
Patients suspected or confirmed to have Nipah virus infection are managed under strict infection-control protocols in healthcare facilities. These include isolation, use of personal protective equipment, and controlled handling of waste and contaminated materials.
Such measures are essential to protect healthcare workers and prevent hospital-based transmission.
Vaccines and future research
At present, there is no licensed vaccine for general public use against Nipah virus. However, several vaccine candidates are under development, and international efforts are ongoing to improve preparedness against potential outbreaks.
Researchers are also studying antiviral therapies and monoclonal antibodies, though these are not yet widely available.
Why Nipah virus remains a global concern
Nipah virus continues to draw attention because of its high fatality rate in past outbreaks, its ability to infect the brain and respiratory system, and the absence of a specific, widely available treatment.
Health experts warn that environmental changes, human encroachment into wildlife habitats, and increased interaction between humans and animals could increase the risk of future spillover events.
For this reason, surveillance, public awareness, and rapid response remain key tools in preventing and controlling Nipah virus outbreaks.